Case Studies
Type I Olecranon Fracture
Dylan Lutter, DVM, DACVS (Large Animal) | Kansas State University
Case Details
Diagnosis and Procedure:
Type I olecranon fracture that had been repaired with pin fixation and a tension band cerclage wire.
The patient developed incisional drainage.
The culture grew a Proteus species sensitive to gentamicin.
Treatment:
Gentamicin 100 mg/ml
Daily dose administered: 10 ml
Treatment duration: 3 days
Outcome: The drainage did improve with use of the Pouch, however, 3 days later the fracture repair failed (bone fragment split) and the owners elected euthanasia.
Vetlen Pouch Assessment: Overall, I found the device quite useful. I really liked the concept, design, placement, and use of the Pouch. I will definitely use the Pouch again, when the time comes.
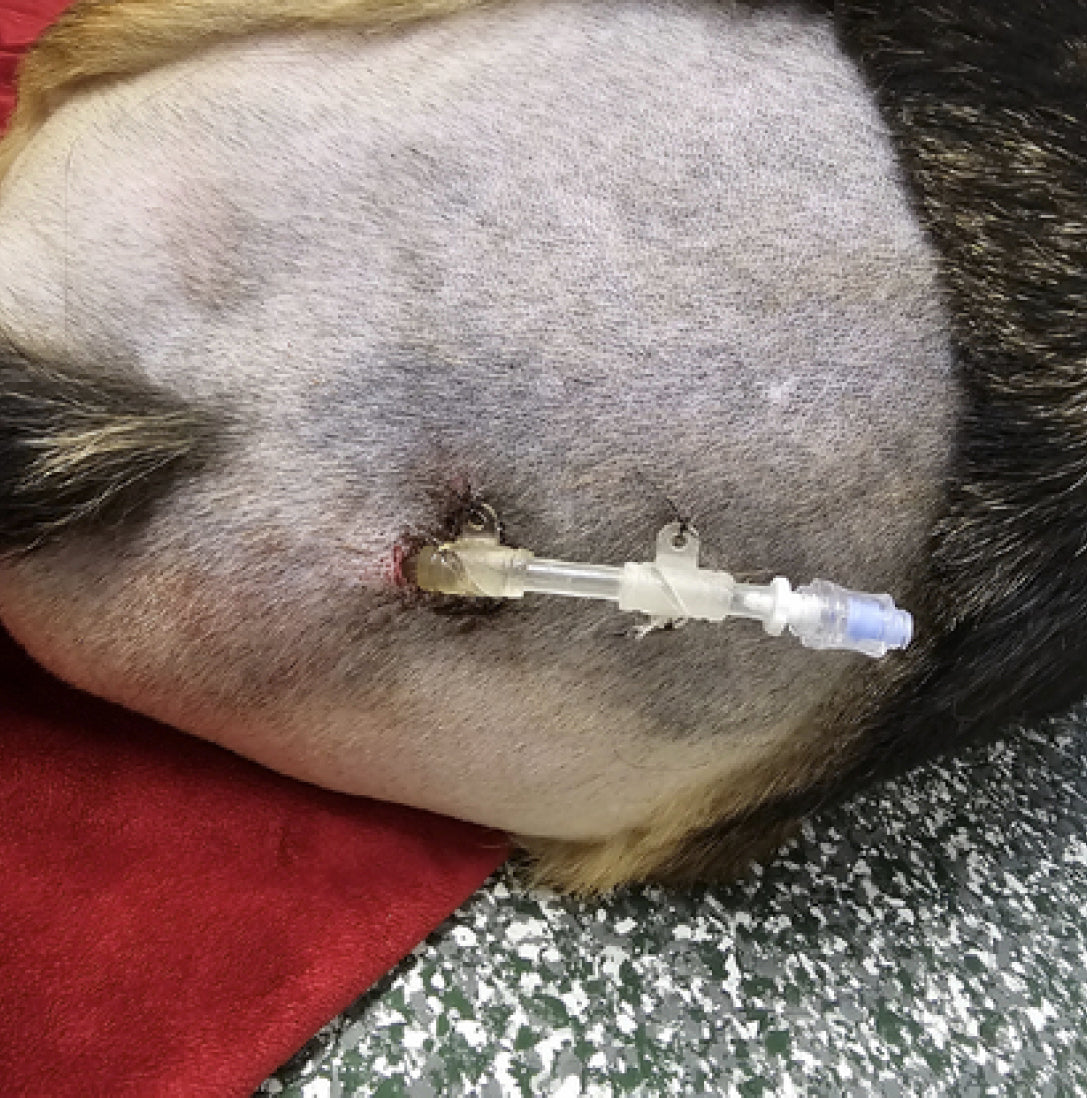
Images




10-days Post Dog Attack
Kaitlyn L. Moss, VMD & Cody P. Doyle, DVM,DACVS (Small Animal) | MedVet Mandeville
Case Details
Patient presented after another dog attacked. The delay in care was due to
the largest snow storm in New Orleans history. Vetlen Pouch was used after
cultures returned with Psuedomonas aeruginosa, staphylococcus
psedintermedius, Bacteroides sp.
Drug & Concentration Used: Amikacin 10mg/kg Pouch q24h for 10 days
Volume of amikacin: 0.43mls (250mg/ml concentration amikacin), diluted 1:1
with sterile saline.
Additional Treatments: Oral marbofloxacin
Treatment Duration: 10 days
Left hindlimb amputation was necessary, the urethra and body wall was saved. Major is living his best life as a three-legged canine!
Product Testimonial: “I cannot say enough nice things about this product. It is a key tool in my toolbox for advanced wound cases,” Dr. Kait Moss.
Images




Left Tibial Tarsal Septic Arthritis
| Rood & Riddle
Case Details
History: Presented for a third episode of non-weightbearing lameness LH, history of two cultures of Staph aureus from the left hock.
Examination: 2/5 Lame at the walk on presentation. Joint aspirate at the farm had 41,000/WBC/ml. Rood & Riddle radiographed her to be sure there had been no trauma and her radiographs were normal. The team changed her to her third antibiotic in IV cefazolin and installed the Vetlen Pouch into her left tibial tarsal joint for five days of intra-articular amikacin.
Prognosis:
Favorable, she went sound after five days and has stayed sound for five days. After consultation the team, we kept her for the finish of her antibiotics because of her history. Her systemic CBC is normal. Her SAA has dropped from 1488 on 5-18-25 to 678 on 5-21-25.
Her hock had less peri-articular swelling and her tibial tarsal effusion is less. There is some fibrosis of the joint portals where she has had all the flushes. Joint fluid aspirate on 5-23-25 WBC is 480/ml with a total protein of 2.1 which are normal.
Treatment: Joint flush, Cefazolin, phenylbutazone, Intra-articular amikacin (10 mL amikacin on 5/14/25, followed by 5 mL amikacin 5/15/25 - 5/18/25.) The Vetlen Pouch was pulled on 5/19/25.
Images

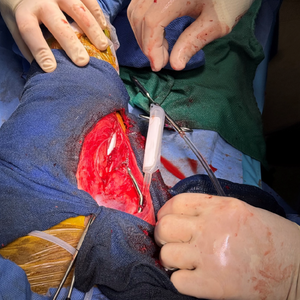
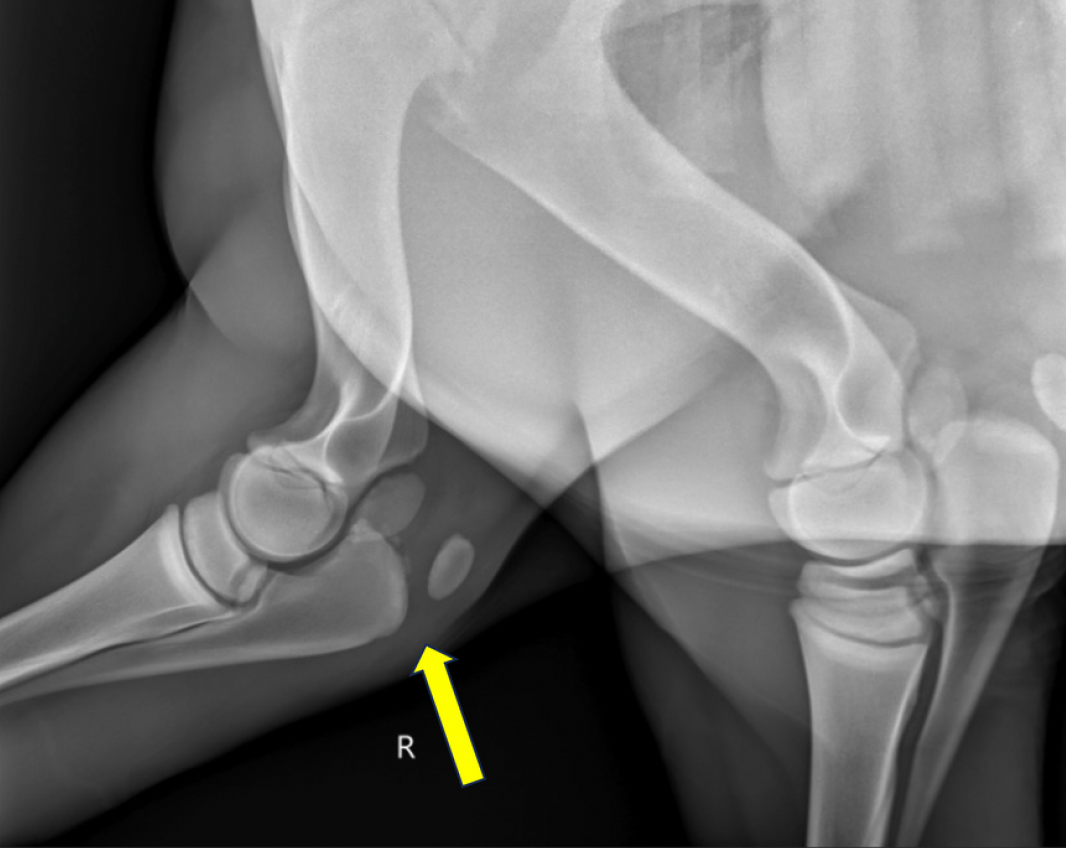
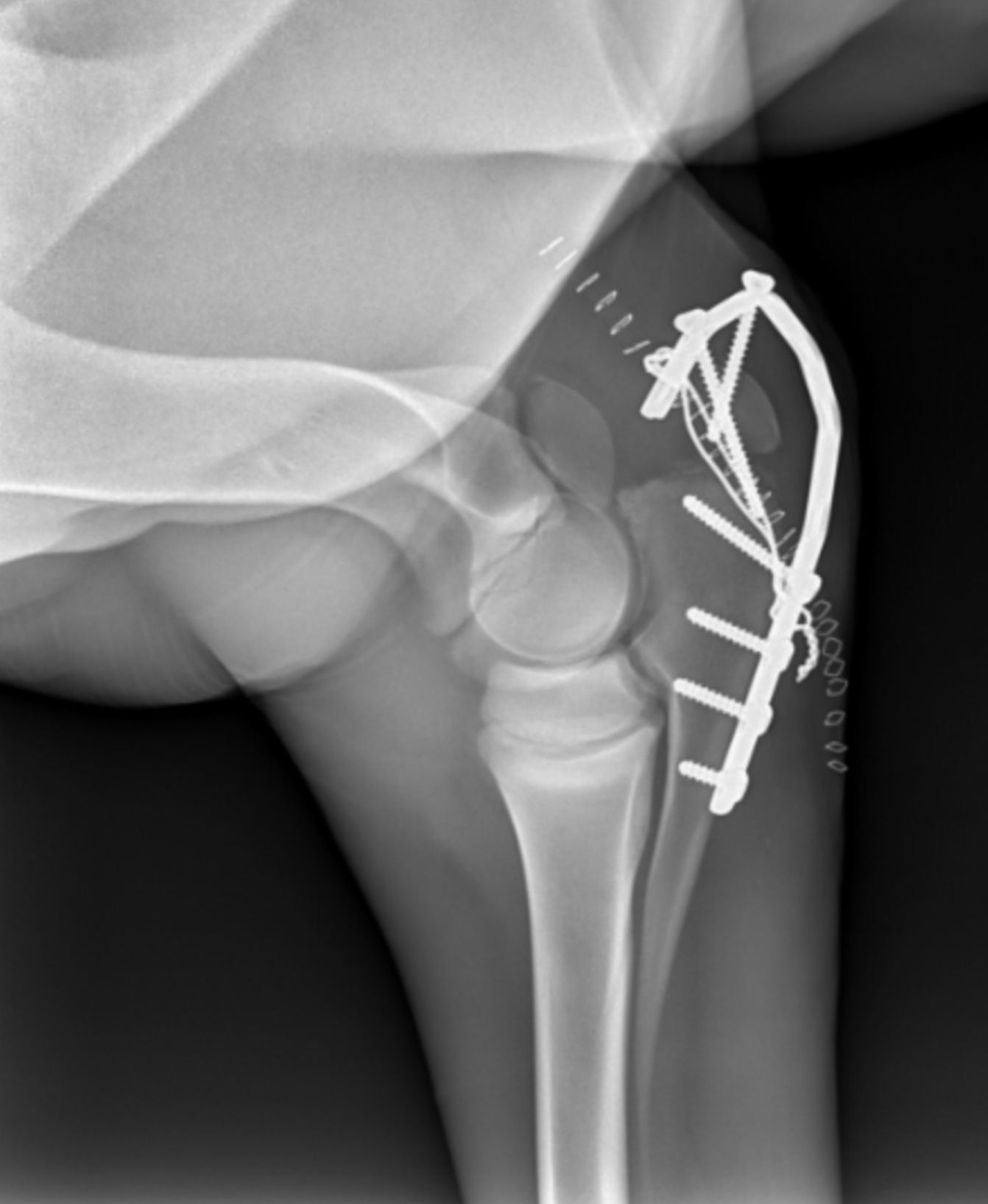
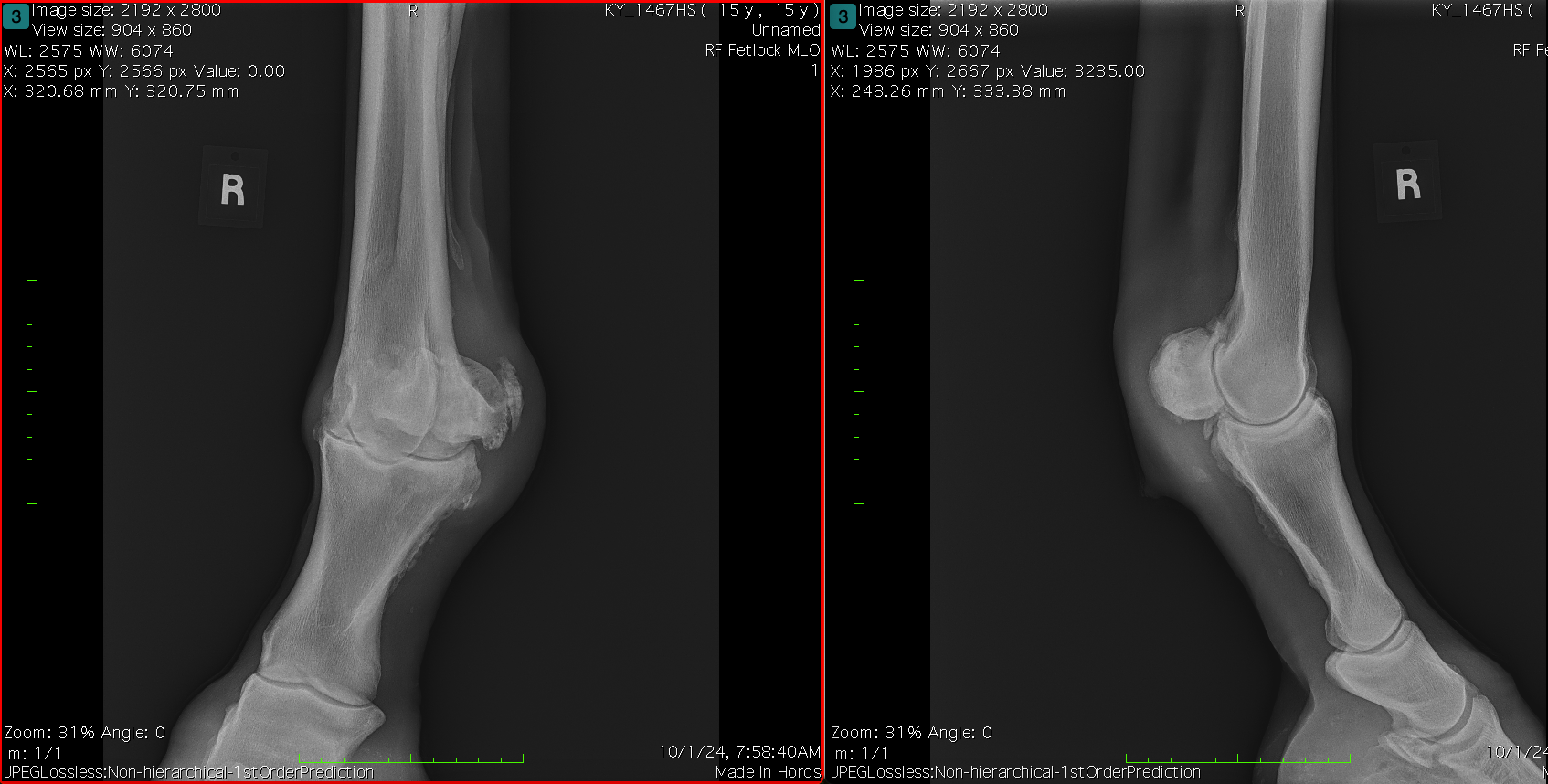
Proximal Ulnar Physeal Fracture
| Rood & Riddle
Case Details
Five-week-old thoroughbred filly diagnosed with a proximal ulnarphyseal fracture. The Vetlen Pouch was used for prophylacticinfection prevention. Ultimately, infection did not occur and thepouch was pulled after four days.
Images




Recurrent Infection of Left Ear Canal Margins Following Total Ear Canal Ablation/Lateral Bulla Osteotomy (TECA-BO) Surgery/TECA Revision
Becky Murray, DVM, DACVS (Small Animal) | Bridge Animal Referral Center (BARC)
Case Details
History and Diagnosis:
Kiki was mauled as a five-week-old kitten and an emergency TECA-BO was performed at the animal shelter by a volunteer veterinarian due to trauma to the region, the left ear pinna was removed as part of this procedure.
After being adopted, Kiki was seen at a different specialty hospital in the area last year to evaluate an abscess on the left cheek. Their exam noted a small ridge of cartilage felt where the base of ear would be and soft swelling on the side of the head. Kiki would scratch the area open and it would drain occasionally. Computer tomography (CT)of the skull showed a deep encapsulated abscess lateral to the osseous bulla. The abscess communicated with the middle ear, within the bulla. Revisional TECA with lateral bulla osteotomy of the left ear was performed and vestibular signs were noted post operatively. She has had multiple courses of antibiotics, including injectable amikacin for the resistant Pseudomonos aeruginosa.
Since then, Kiki has had recurrent draining tracts/abscesses at her TECA-BO with multi-drug resistant bacterial on culture results. Kiki was first seen at BARC on March 18, 2025 for a CT. The CT showed a 6.8mm x 7.8mm region of rim-enhancing tissue at the base of the left ear just lateral to the tympanic bulla suggesting a region of persistent infection/inflammation, with some inflammation extending lateral to the region. No cutaneous drainage was noted at the time of CT.
A third surgery was recommended for further debridement of the region and 5 mL Vetlen Pouch placement. Since the clients had difficulty with all oral medications, an esophagostomy feeding tube was also recommended.
Surgery:
A dorsal to ventral ellipse was performed to remove a section of the previous TECA incision as well as active 3mm draining tract. Sharp and blunt dissection was used to follow the scar tissue/inflammatory tissue deep to its attachment to the external acoustic meatus. The remaining annular cartilage/tissue was freed from the bulla with a freer elevator and sharp dissection. A lateral bulla osteotomy was performed, purulent discharge “exploded” from the bulla once entered. All diseased tissues and secretory linings were removed from within the bulla with gentle curettage. A culture of the bulla was taken at the end of the procedure post-lavage. Culture results ultimately confirmed continued Pseudomonas infection, sensitive to amikacin.
A 5mL Vetlen Pouch was placed superficial to the region. The pouch was very stiff and could not be folded down into the area, but seemed to sit well in the SQ space of the facial region. A single 3-0 Prolene was used to secure the distal tip of the pouch to the skin on the ventral mandibular region. Using the provided trocar, the tubing was exited out the dorsal cervical region, trimmed down to a manageable length and secured with 3-0 Prolene. The subcutaneous tissues and skin were then closed routinely superficial to the pouch.
Clients were taught to use the pouch once daily to administer 15mg/kg of amikacin diluted in 4 mL of saline. Clients found the product easy to use and Kiki tolerated the instillation process much better than previous injections or oral drug administration. The Vetlen Pouch was removed under sedation at two and a half weeks, skin incision healed routinely. The exit site was larger than typical for e-tube and it was partially apposed with suture. Client went to their primary veterinarian for suture removal and report that Kiki is in good spirits with a great appetite and no new concerns noted.
Images



Degloving Injury of Left Tarsometarsal Region, Resulting in Skin Sloughing and Mixed Bacterial Infection
Toni L. Trego, DVM | Amboy Vet Clinic
Case Details
Patient Signalment: 5-Year-Old Male Neutered Shih Tzu
Diagnosis: Degloving Injury of Left Tarsometarsal Region, Resulting in Skin Sloughing and Mixed Bacterial Infection
History & Diagnosis: The dog was presented on 3/3/25 immediately following vehicular trauma to his left hind leg. Remarkably, no bony injuries were identified. However, the skin had been avulsed from the underlying tissue, extending from just proximal to the hock down to the toes. After several days of conservative management — including a drain, bandaging, oral antibiotics, and pain medication — all of the affected skin sloughed. A culture was obtained at the time of debridement on 3/10/25.
Implantation March 12, 2025: A pouch flap was created on the left body wall, and the left hind leg was inserted into the flap and sutured in place, along with a fenestrated drain and a 10 mL Vetlen Pouch. The drain was removed on 3/15/25. Antibiotic treatment administered through the pouch. The client was very grateful to discontinue oral antibiotics once the switch to vancomycin was made, as administering oral medications to the patient had been challenging.
Drug and Concentration used in the Vetlen Pouch: Initially ceftiofur sodium, 50 mg dose, qs to 9 mL total volume with 0.9% NaCl (3/12/25 through 3/21/25). Culture results revealed multi-drug resistant Enterococcus faecium along with Streptococcus canis and Staphylococcus schleiferi, so the doctor switched tovancomycin hydrochloride, 30mg dose, qs to 6ml total volume with 0.9% NaCl(3/22/25 through 4/1/25).
Explantation April 2, 2025: The flap of skin was excised from the donor site and was closed over the left distal limb. The Vetlen Pouch was removed, discarded, and the body wall wound was closed routinely. Parts of the flap became necrotic and sloughed; however, the majority has survived with only small areas of open granulating wounds currently remaining. As of today's bandage change, healing is progressing well, and the client is delighted with the result.
Images





Torn Left Hind Achilles
Amanda Conkling, DVM, DACVS (Small Animal) | BluePearl Pet Hospital Grand Rapids
Case Details
History:
Dog diagnosed with probable torn Achilles in March and treated with Gabapentin and Galliprant. Dog had previously torn CCL on RH and has a history of seizures. Toe touching lameness progressed into flattening of the left hind limb and dog was referred for potential surgical correction.
Diagnosis:
- Achilles tendon rupture – left complete, degenerative, possibly early right degeneration
- Cranial cruciate ligament tear – right extracapsular stabilization with persistent instability
Surgical Treatment Timeline:
The tendon was debrided and repaired by reattaching to the calcaneous. The repair site was wrapped in porcine collagen sheeting and injected with PRP to aid in healing. A screw was placed from calcaneous into tibia/fibula to maintain the tarsus in extension. Cast placed, recheck in one week.
9 Days Post-op: Grade III/IV lame in left and right rear limbs. Left cast in place, purulent discharge noted from incision. Culture obtained and cast replaced with a mepilex bandage. Right stifle remains unstable.
Culture confirmed surgical site infection, patient prescribed Baytril and Chloramphenicol. Bandage was intact and incision was intact with serosanguinous drainage. Calcaneal tendon and tibiocalcaneal screw palpated stable.
21 Days Post-op: Surgical site infection persisted and patients experienced intermittent vomiting and reduced appetite. Chloramphenicol discontinued and replaced with amikacin 750mg SC SID for 10 days.
36 Days Post-Achilles Repair: Dog underwent TPLO surgery for right hind CCL repair.
42 Days Post-Achilles Repair: A draining tract was present on the lateral aspect of the tarsus and the tissue around it was swollen. Culture taken and radiographs revealed lysis of the calcaneus due to suspected osteomyelitis. The tibiocalcaneal screw was intact. Amikacin 750mg SC SID prescribed.
47 Days Post-Achilles Repair:
Implant removed and Kerrier beads placed
Calcaneal screw was removed, screw was loose. Tendon palpated intact with sutures and discolored periseal visualized. Numerable amikacin Kerrier beads placed in the screw tract and around the site to capacity. Cast replaced.
15 Days Post-Bead Placement, 62 Days Post-Achilles Repair: Cast removed with marked malodorous discharge from proximal incision, purulent with beads being extruded. Culture obtained, site cleaned, and honey bandage placed with lateral component of splint. Owner advised if infection cannot be controlled, aggressive debridement and long-term support via custom orthotic or pantarsal arthrodesis once infection is 100% cleared.
43 Days Post-Bead Placement, 90 Days Post-Achilles Repair: Multiple rechecks over the last 30 days show persistent infection with the Kerrier beads extruding. Grade III/IV lame left rear limb with plantigrade stance and persistent purulent discharge from proximal aspect of the lateral hock incision and strike through on the bandage. Recommend custom orthotic brace and re-cultured to determine treatment plan.
48 Days Post-bead Placement, 95 Days Post-Achilles Repair
Vetlen Pouch Placement to Treat MSRP Infection and Implant Removal
Under brief anesthesia, a lateral approach to the left Achilles was performed. The previously placed periseal and all identifiable prolene sutures were removed. Copious lavage and sponge debridement. A Vetlen Pouch was placed and the tube exited proximal lateral tibia. Pouch secured via 3-0 PDS distal tacking suture and tube secured via tacking sutures. Site closed via 3-0 PDS SC and skin staples. Vetlen Pouch doses with 750 mg of amikacin daily.
15 Days Post- Vetlen Pouch Placement: The pouch was removed without incident, with some of the pouch already migrating out of the wound.
11 Weeks Post Implant Removal: Grade I/IV lame, patient stable with custom orthotic. No sign of infection.
Assessment: The Vetlen Pouch was very easy to place (similar to any JP drain) and simple for owners to use at home with the daily injections. It was very well tolerated by the dog in this case.
Images






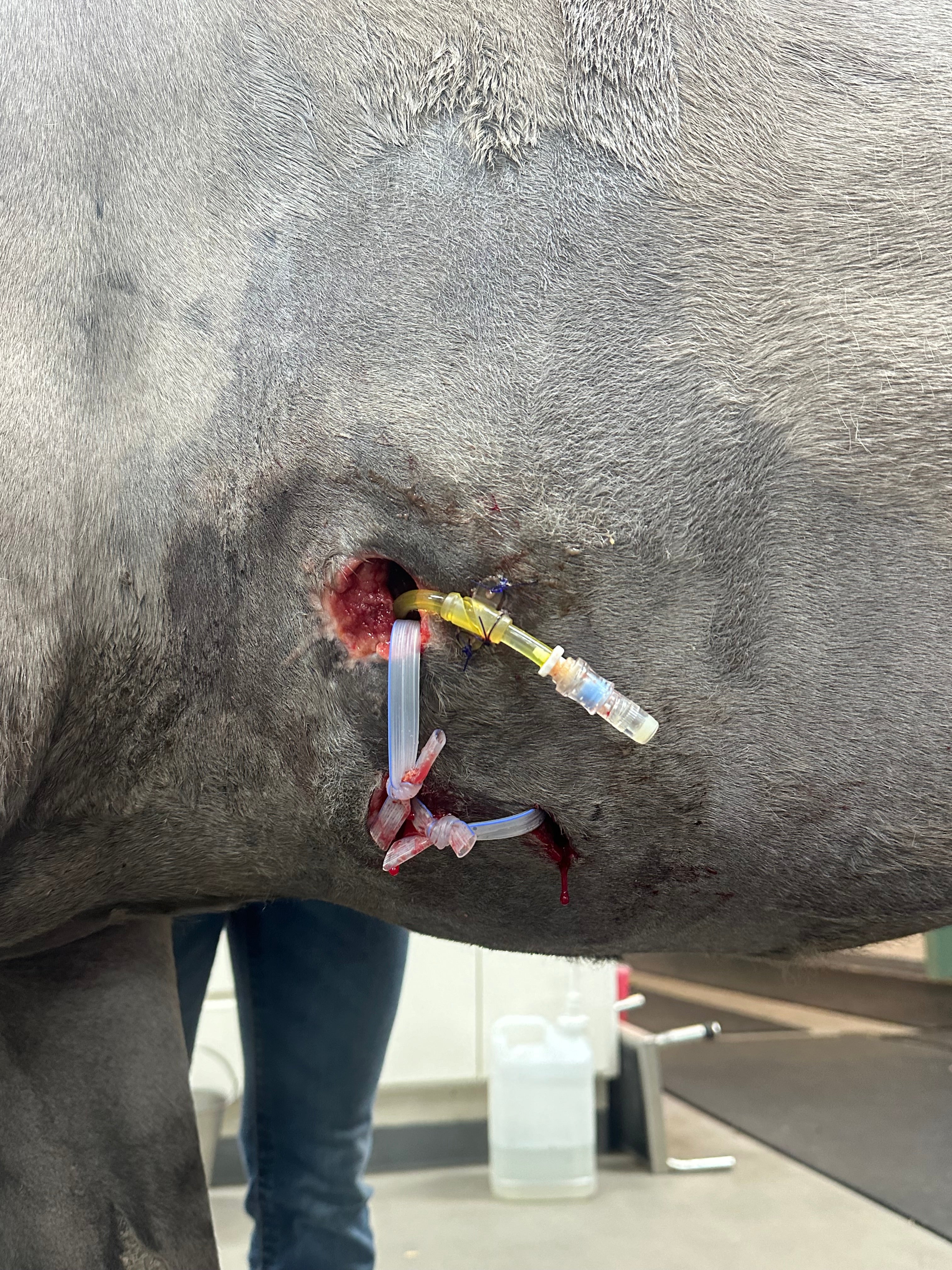
Thoracic Puncture Wound Leading to Splenic Abscess
Karen Blake, DVM, DIPL. ACVS (Large Animal) | Bend Equine Medical Center
Case Details
Patient Signalment: Two-Year-Old Mustang
Diagnosis: Thoracic Puncture Wound Leading to Splenic
Abscess
Treatment: Vetlen Pouch placed inside wound and treated with
10 mL ceftiofur every 24 hours for 4 days.
Outcome: Response to Vetlen Pouch for this case was impressive.
Images


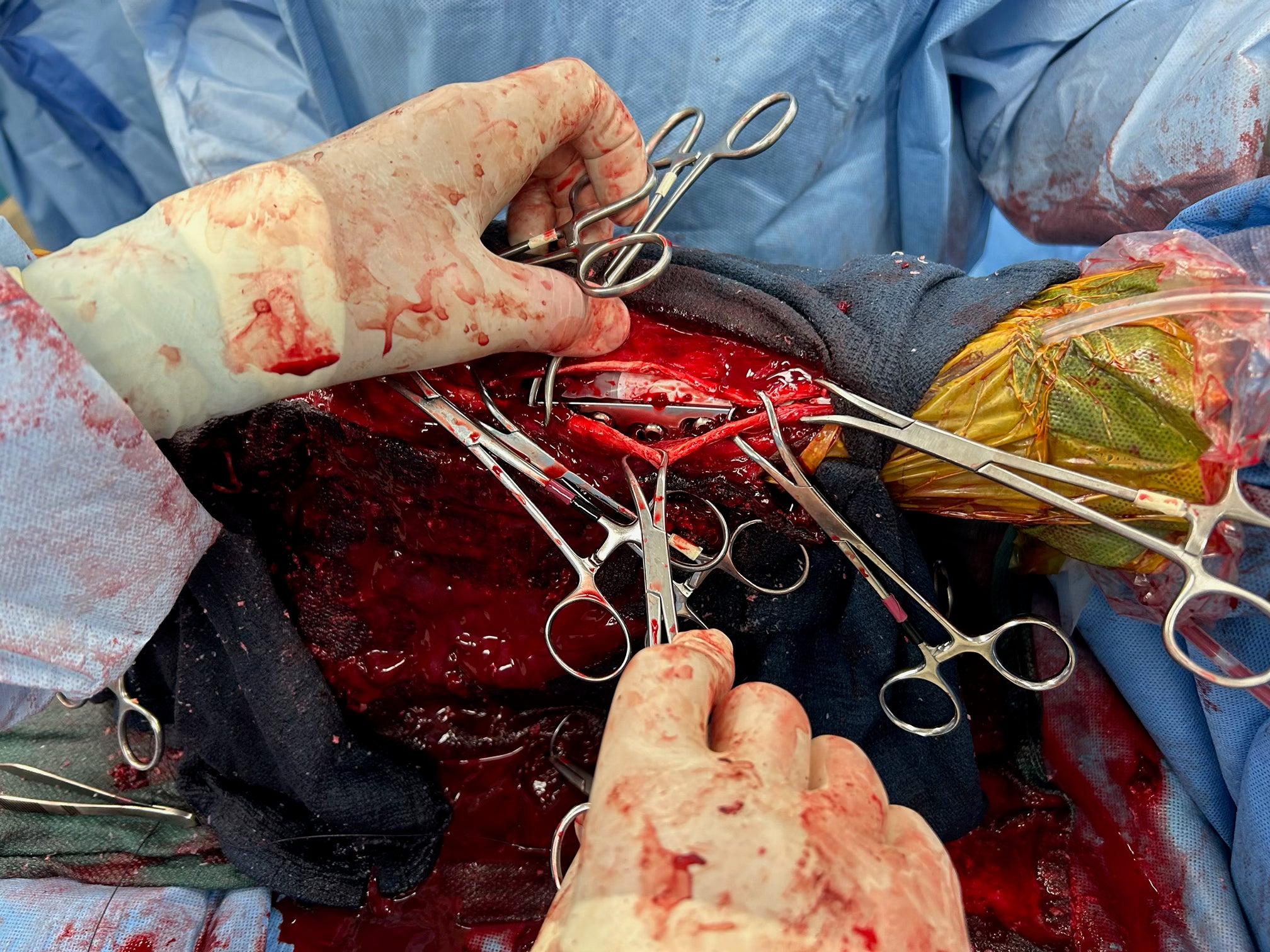
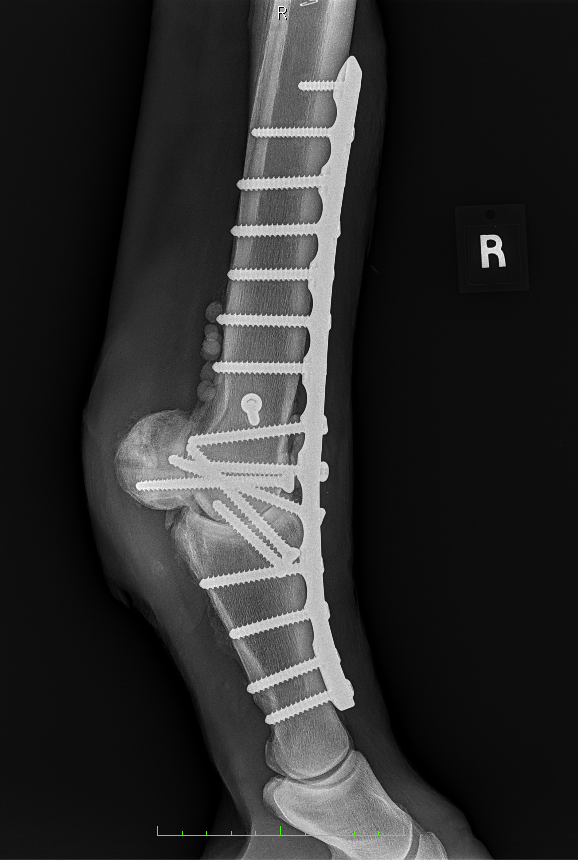
Fetlock Arthrodesis Due To Degenerative Arthritis
| Rood & Riddle
Case Details
Diagnosis and Procedure: Degenerative arthritis of the fetlock joint, pain leading to overloading the other foot. Fetlock arthrodesis was performed.
Treatment:
Amikacin 250 mg/ml
Daily dose administered: 6 ml
Days of treatment: 5 days
Conclusion: Vetlen Pouch worked well. The surgeon liked the ability to instill the antibiotics onto the plate for 5-days post-op. The mare has done well and is back home.
Images


Infected Supraspinous Bursa (Fistulous Withers)
Lindsay Knott, DVM | Loomis Basin Equine Medical Center
Case Details
Patient Signalment: Six-Year-Old Quarter Horse Gelding
Diagnosis: Infected Supraspinous Bursa (Fistulous Withers)
INITIAL SURGERY
Diagnosis and Procedure:
Current case is an infected supraspinous bursa, failed medical management. Resection of the affected nuchal ligament and bursa performed after about four weeks of medical management. Picture of wound prior to pouch placement on December 16, 2023.
- Antibiotic prescribed: Amikacin 250 mg/ml
- Daily dose administered: 5 ml
- Days of treatment: 26 days
- Additional treatments: Ceftiofur sodium and gentamicin systemically dosed for the first 16 days of treatment.
- Culture result: A very resistant Enterobacter cloacae susceptible to amikacin and imipenem.
Vetlen Pouch Explanation
Infused 20 ml lidocaine (two percent) one hour prior to removal, and mildly sedated the patient at time of removal. The pouch came out seamlessly without any issues and was a very painless experience for both the patient and doctor.
Vetlen Pouch Assessment
The Vetlen Pouch allowed for targeted antimicrobial therapy when dealing with a deep surgical site infection, which cultured a multi-drug-resistant bacteria. Systemic administration of the necessary antimicrobial would have been extremely cost prohibitive, and the pouch allowed for easy, daily dosing (once) at a much smaller, but locally effective volume. Additional wound care and treatment of the surgical site was also possible while leaving the pouch in situ. I would absolutely consider the use of this product for other cases in the future.
Images



Chronic Multi-drug Resistant Wound (> 1 year) Lateral to Anus
Hayley Gallaher, DVM, MS, DACVS (Small Animal) | Michigan State University
Case Details
Patient Signalment: Seven-year-old Male (Neutered) German Shepherd
Diagnosis: Chronic multi-drug resistant wound (> 1 year) lateral to anus
INITIAL SURGERY
History and Vetlen Pouch Placement:
- The patient presented with a chronic wound of greater than one year lateral to the anus. This is not a perianal fistula.
- Culture shows multi-drug resistance (MDR) Staphylococcus pseudointermedius.
- Due to the location, closure rather than open wound management was desirable.
- The Vetlen Pouch was placed on April 19, 2024.
- Treated with Amikacin – 5 mL @ 250 mg/mL for 1 week.
Assessment:
The Vetlen Pouch offers an additional option for longer-term administration. The pouch was great for this patient as it spared them the potential adverse effects from systemic administration. The Vetlen Pouch was removed on April 26, 2024.
The patient healed well and there has been no recurrence.
Images




Right Hind Dorsal Fetlock Laceration and Trauma
| Rood & Riddle
Case Details
Patient Signalment: Nine-year-old Quarter Horse Mare
Diagnosis: Right Hind Dorsal Fetlock Laceration and Trauma
INITIAL SURGERY
Diagnosis and Procedure (April 3, 2024):
Mare presented with a severe right hind dorsal fetlock laceration and trauma. The injury included torn joint capsule transected digital extensor tendon. surgical intervention included:
- Surgical debridement: Removal of damaged tissue to prevent infection.
- Regional limb perfusion: Infusion of 500 mg of Meropenem and 60 cc of saline to deliver antibiotics directly to the affected area.
- Fetlock joint lavage: Cleansing of the joint using Povidone-Iodine in Lactated Ringer’s.
- Vetlen Pouch placement: Dosed with 9 ml Amikacin (250 mg/ml) daily.
- Wound closure: Skin laceration was closed, although much of the subcutaneous tissue was too damaged to repair fully.
Assessment: Despite the extensive trauma, including a shredded extensor tendon and avulsed joint capsule, initial surgery aimed to stabilize the limb and minimize infection. A cast was applied to immobilize the fetlock, critical for healing given the tissue damage. The Vetlen Pouch's efficacy would be monitored, and the cast might be changed based on the mare’s comfort and healing progress.
Follow-Up Examination & Vetlen Pouch Explantation (April 18, 2024) Examination Findings:
- Healing status: The wound and joint capsule were healing well with minimal skin loss.
- Lameness: 5/5 Lame initially post-injury.
- Suture removal and cast change: The wound showed favorable healing, indicating effective management of infection and tissue repair.
Prognosis and Recommendations: The extensor tendon typically requires 3-4 months for functional healing. The next cast change was scheduled for May 1st, transitioning to a bandage cast and eventually a splint to protect the fetlock from excessive flexion.
Follow-Up Examination (May 2, 2024)
Four weeks post-trauma, mare showed significant healing of the fetlock joint capsule avulsion, long digital extensor tendon transection, and dorsal fetlock laceration.
Examination Findings:
- Lameness: 0/5 Lame at the walk, indicating significant improvement.
- Wound condition: Healthy granulation tissue filled the wound, though some skin loss due to disrupted blood supply was noted.
- Radiographs: Normal, with no bone or joint damage.
- Cast change: Transitioned from an immobilizing cast to a bandage cast to allow controlled motion while preventing excessive flexion.
Prognosis and Recommendations: The prognosis remained favorable. Continued stall rest and careful monitoring were advised. The bandage cast would be split into a splint in one week to protect the healing tendon. The support shoe on the left hind foot would remain for another 1-2 weeks. Hand grazing would commence in two weeks, with targeted purposeful walking starting two months post-injury.
Future Management: Mare’s recovery trajectory was positive, with careful management ensuring the tendon and joint capsule heal without complications. Monitoring for any signs of infection or discomfort remained crucial, with adaptive treatment based on her progress.
Conclusion: Mare’s case demonstrates the potential of the Vetlen Pouch in managing severe equine wounds by providing sustained local antibiotic delivery. Her recovery, though complex, highlights the importance of innovative veterinary devices in improving treatment outcomes for traumatic injuries.
Images