Resources
Case Studies

Recurrent Infection of Left Ear Canal Margins Following Total Ear Canal Ablation/Lateral Bulla Osteotomy (TECA-BO) Surgery/TECA Revision
Becky Murray, DVM, DACVS | Bridge Animal Referral Center (BARC)
Case Details
History and Diagnosis:
Kiki was mauled as a five-week-old kitten and an emergency TECA-BO was performed at the animal shelter by a volunteer veterinarian due to trauma to the region, the left ear pinna was removed as part of this procedure.
After being adopted, Kiki was seen at a different specialty hospital in the area last year to evaluate an abscess on the left cheek. Their exam noted a small ridge of cartilage felt where the base of ear would be and soft swelling on the side of the head. Kiki would scratch the area open and it would drain occasionally. Computer tomography (CT)of the skull showed a deep encapsulated abscess lateral to the osseous bulla. The abscess communicated with the middle ear, within the bulla. Revisional TECA with lateral bulla osteotomy of the left ear was performed and vestibular signs were noted post operatively. She has had multiple courses of antibiotics, including injectable amikacin for the resistant Pseudomonos aeruginosa.
Since then, Kiki has had recurrent draining tracts/abscesses at her TECA-BO with multi-drug resistant bacterial on culture results. Kiki was first seen at BARC on March 18, 2025 for a CT. The CT showed a 6.8mm x 7.8mm region of rim-enhancing tissue at the base of the left ear just lateral to the tympanic bulla suggesting a region of persistent infection/inflammation, with some inflammation extending lateral to the region. No cutaneous drainage was noted at the time of CT.
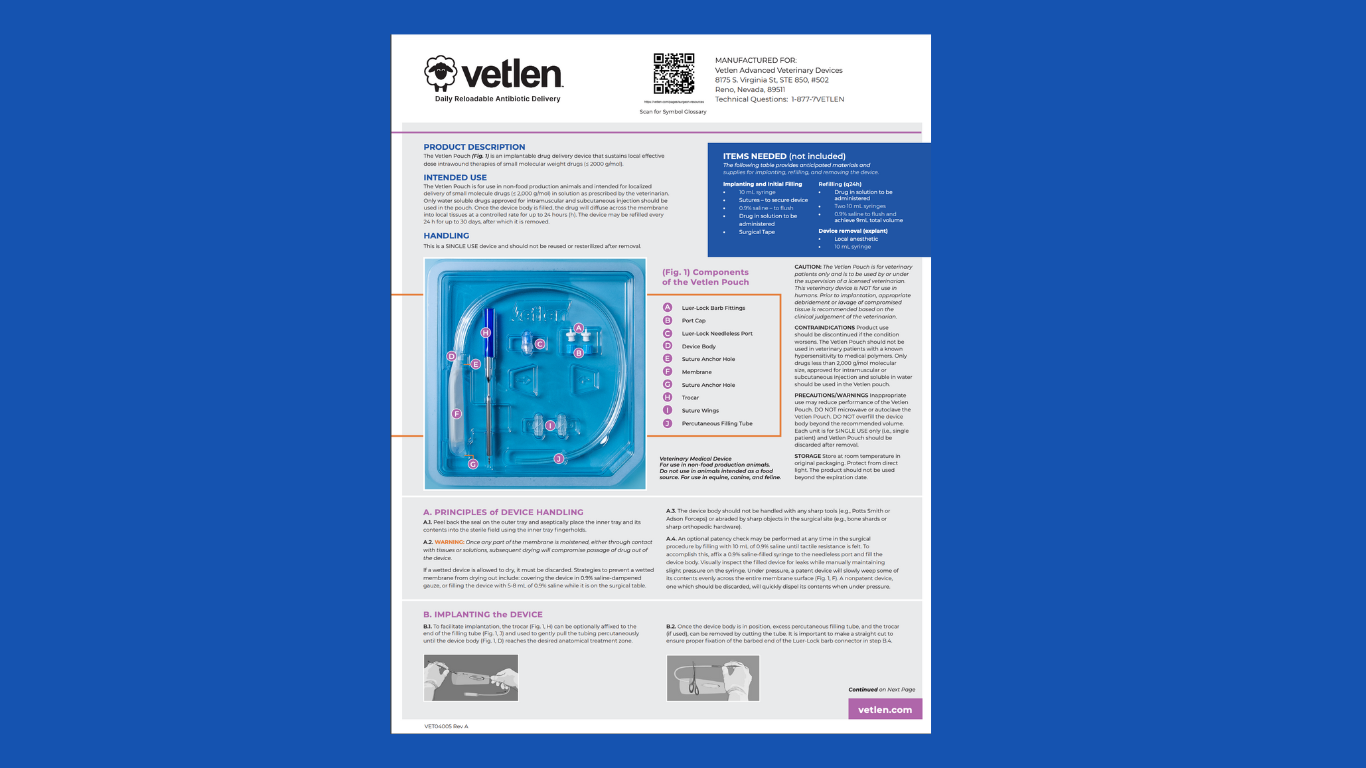
A third surgery was recommended for further debridement of the region and 5 mL Vetlen Pouch placement. Since the clients had difficulty with all oral medications, an esophagostomy feeding tube was also recommended.
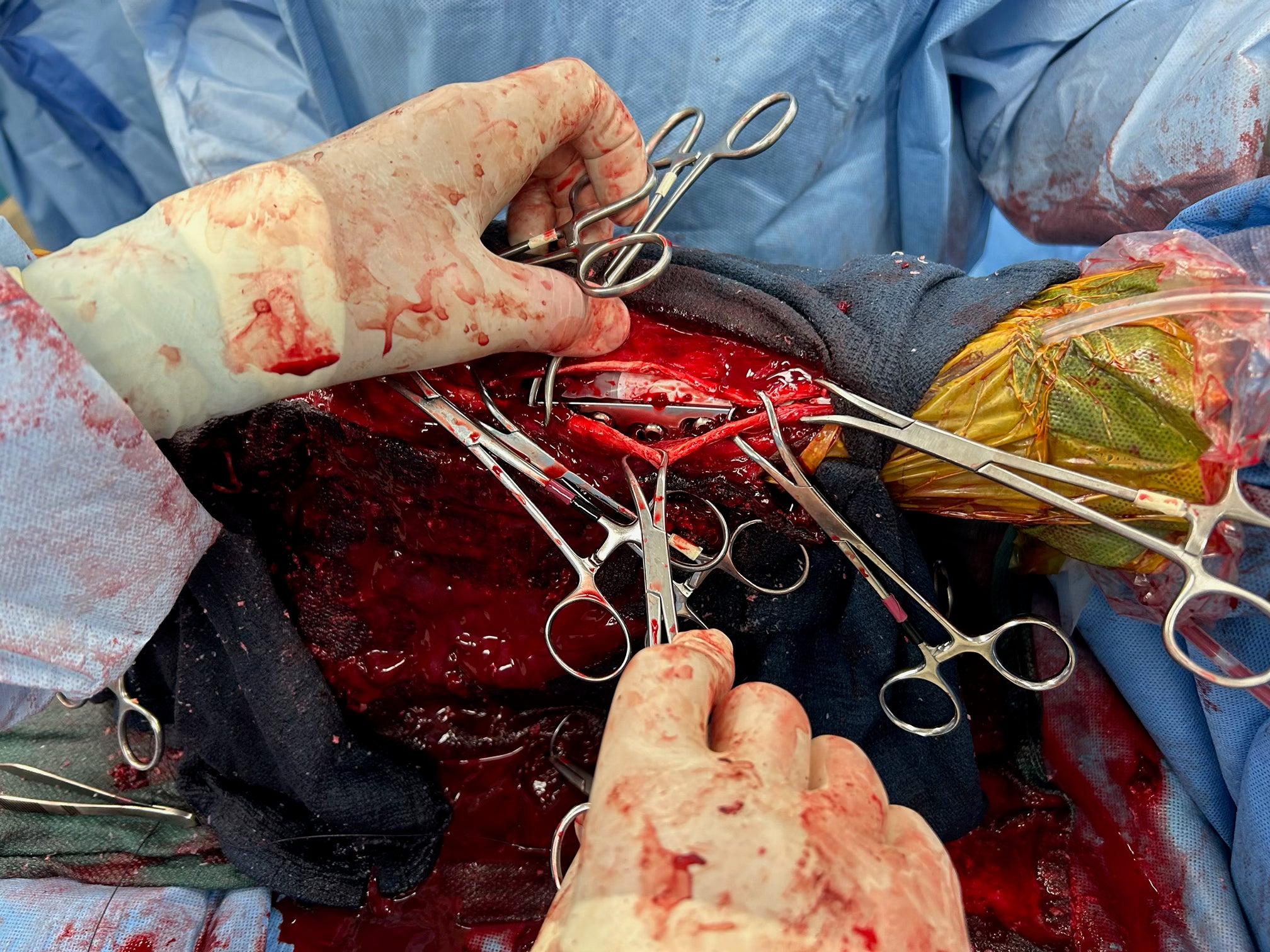
Surgery:
A dorsal to ventral ellipse was performed to remove a section of the previous TECA incision as well as active 3mm draining tract. Sharp and blunt dissection was used to follow the scar tissue/inflammatory tissue deep to its attachment to the external acoustic meatus. The remaining annular cartilage/tissue was freed from the bulla with a freer elevator and sharp dissection. A lateral bulla osteotomy was performed, purulent discharge “exploded” from the bulla once entered. All diseased tissues and secretory linings were removed from within the bulla with gentle curettage. A culture of the bulla was taken at the end of the procedure post-lavage. Culture results ultimately confirmed continued Pseudomonas infection, sensitive to amikacin.
A 5mL Vetlen Pouch was placed superficial to the region. The pouch was very stiff and could not be folded down into the area, but seemed to sit well in the SQ space of the facial region. A single 3-0 Prolene was used to secure the distal tip of the pouch to the skin on the ventral mandibular region. Using the provided trocar, the tubing was exited out the dorsal cervical region, trimmed down to a manageable length and secured with 3-0 Prolene. The subcutaneous tissues and skin were then closed routinely superficial to the pouch.
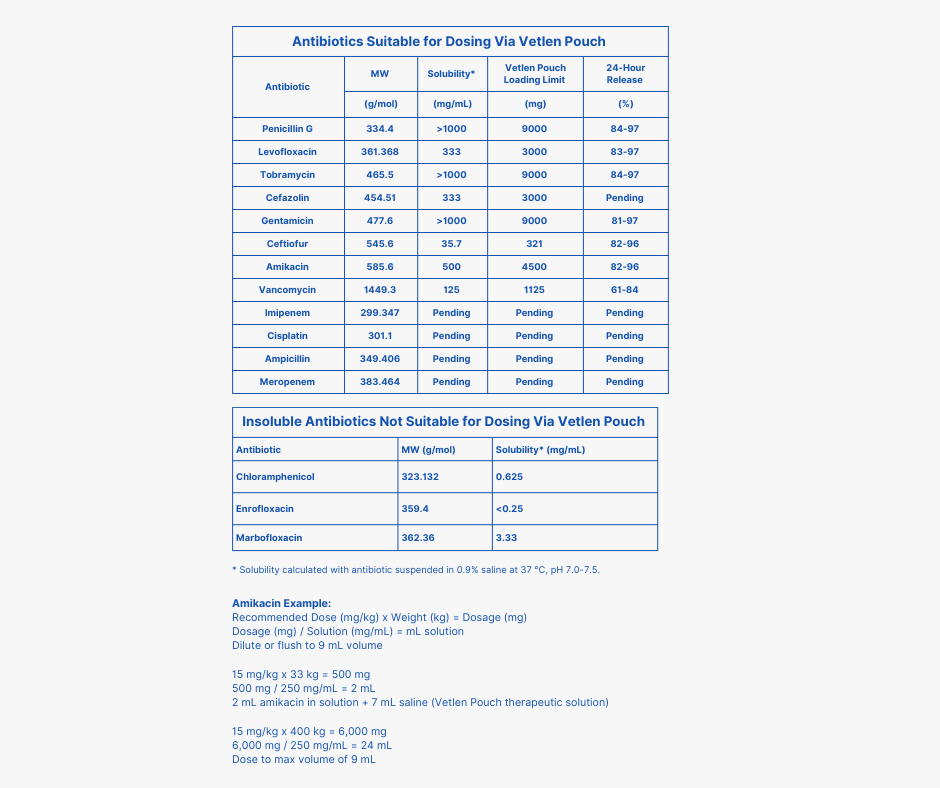
Clients were taught to use the pouch once daily to administer 15mg/kg of amikacin diluted in 4 mL of saline. Clients found the product easy to use and Kiki tolerated the instillation process much better than previous injections or oral drug administration. The Vetlen Pouch was removed under sedation at two and a half weeks, skin incision healed routinely. The exit site was larger than typical for e-tube and it was partially apposed with suture. Client went to their primary veterinarian for suture removal and report that Kiki is in good spirits with a great appetite and no new concerns noted.
Images




Degloving Injury of Left Tarsometarsal Region, Resulting in Skin Sloughing and Mixed Bacterial Infection
Toni L. Trego, DVM | Amboy Vet Clinic
Case Details
Patient Signalment: 5-Year-Old Male Neutered Shih Tzu
Diagnosis: Degloving Injury of Left Tarsometarsal Region, Resulting in Skin Sloughing and Mixed Bacterial Infection
History & Diagnosis: The dog was presented on 3/3/25 immediately following vehicular trauma to his left hind leg. Remarkably, no bony injuries were identified. However, the skin had been avulsed from the underlying tissue, extending from just proximal to the hock down to the toes. After several days of conservative management — including a drain, bandaging, oral antibiotics, and pain medication — all of the affected skin sloughed. A culture was obtained at the time of debridement on 3/10/25.
Implantation
March 12, 2025: A pouch flap was created on the left body wall, and the left hind leg was inserted into the flap and sutured in place, along with a fenestrated drain and a 10 mL Vetlen Pouch. The drain was removed on 3/15/25. Antibiotic treatment administered through the pouch. The client was very grateful to discontinue oral antibiotics once the switch to vancomycin was made, as administering oral medications to the patient had been challenging.
Drug and Concentration used in the Vetlen Pouch: Initially ceftiofur sodium, 50 mgdose, qs to 9 mL total volume with 0.9% NaCl (3/12/25 through 3/21/25). Cultureresults revealed multi-drug resistant Enterococcus faecium along with Streptococcus canis and Staphylococcus schleiferi, so the doctor switched tovancomycin hydrochloride, 30mg dose, qs to 6ml total volume with 0.9% NaCl(3/22/25 through 4/1/25).
Explantation
April 2, 2025: The flap of skin was excised from the donor site and was closed over the left distal limb. The Vetlen Pouch was removed, discarded, and the body wall wound was closed routinely. Parts of the flap became necrotic and sloughed; however, the majority has survived with only small areas of open granulating wounds currently remaining. As of today's bandage change, healing is progressing well, and the client is delighted with the result.
Images







Fetlock Arthrodesis Due To Degenerative Arthritis
| Rood and Riddle
Case Details
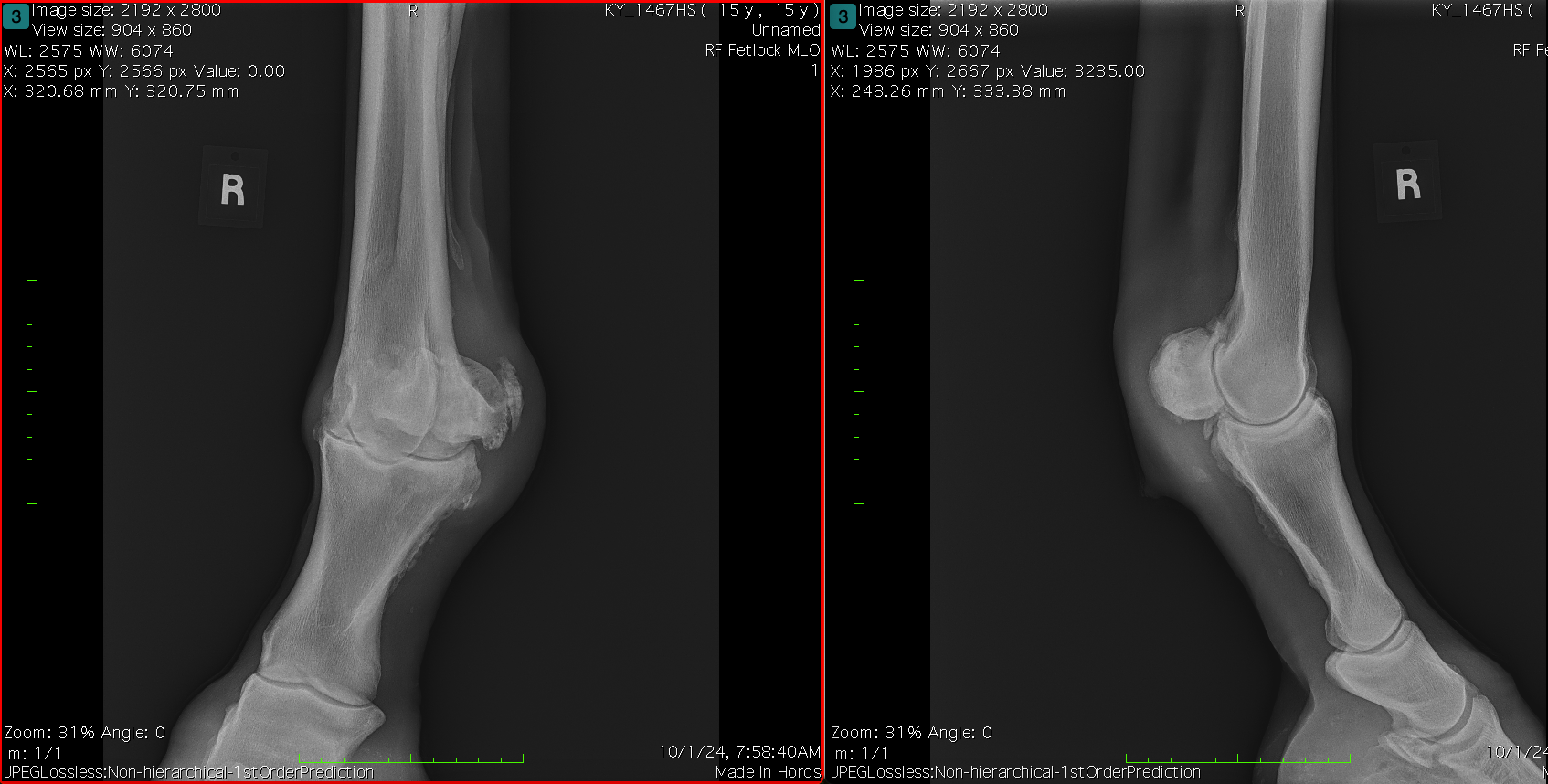
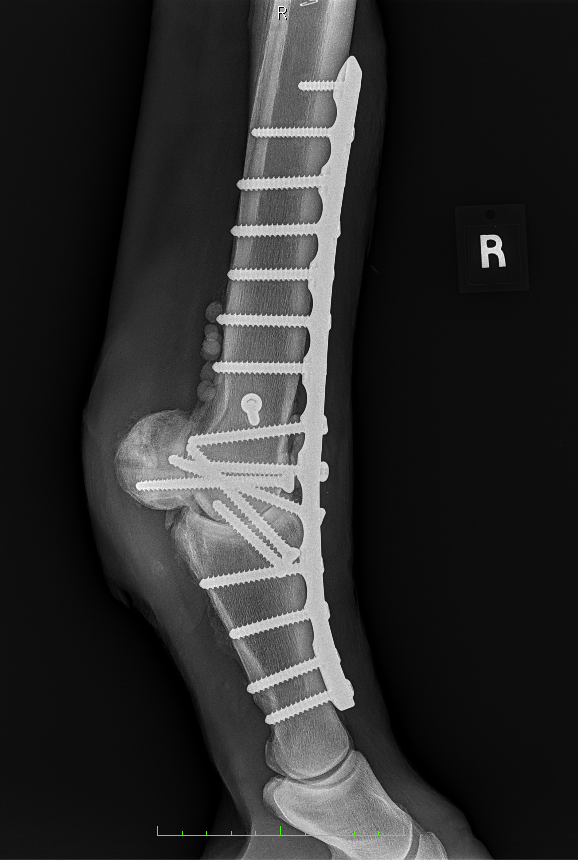
Diagnosis and Procedure: Degenerative arthritis of the fetlock joint, pain leading to overloading the other foot. Fetlock arthrodesis was performed.
Treatment:
Amikacin 250 mg/ml
Daily dose administered: 6 ml
Days of treatment: 5 days
Conclusion: Vetlen Pouch worked well. The surgeon liked the ability to instill the antibiotics onto the plate for 5-days post-op. The mare has done well and is back home.
Images